Background Information of Parkinson’s Disease
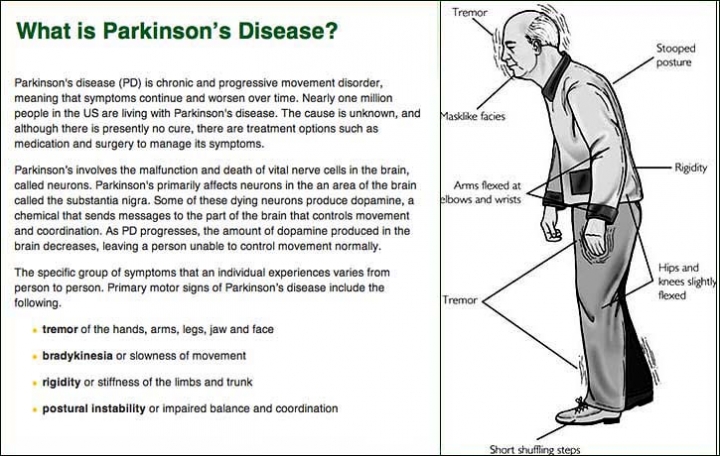
James Parkinson described Parkinson’s Disease as a mental disorder that forces body parts into involuntary tremors . According to Lorraine V. Kalia and Anthony E. Lang, the leading cause for developing PD is death of dopaminergic neurons in the Substantia Niagara leading to a deficiency of dopamine in the Basal Ganglia
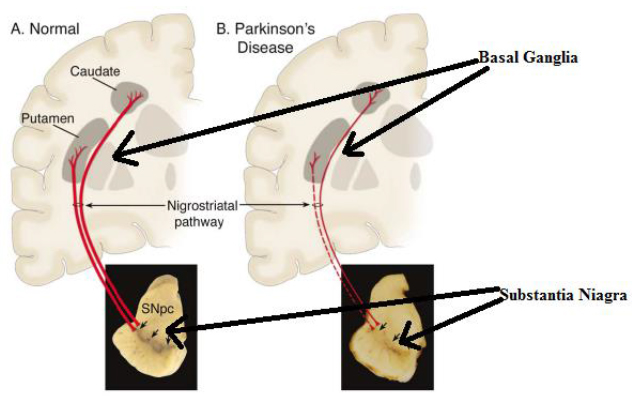
FIGURE 1. Comparison of normal brain and a brain of patient suffering from PD
Figure 1 illustrates the Substantia Niagara and the Basal Ganglia, of a normal person compared to a PD affected patient. Substantia Niagara and the Basal Ganglia are located in middle brain. As observed by Lanneke M.L. deLau and Monique M.B. Breteler, the Substantia
Niagara produces the dopamine, which is used by the Basal Ganglia. The Basal Ganglia contains the Putamen and the Caudate, which controls motor functions. The red lines shown in Figure 1 are the nerves transferring dopamine from the Substantia Niagara to the Basal Ganglia. The dotted red line represents the reduced flow of dopamine in patient affected by Parkinson’s Disease. According to the theory proposed by William Dauer and Serge Przedborski, motor neurons will transmit a false signal to various parts of the body. This false signal will produce an involuntary movement with a seemingly fixed frequency . In addition to the involuntary movement the major cause for the onset of Parkinson’s Disease is the collection of protein (brown spot) in Substantia Niagara called Lewy bodies as observed in Figure 2. Due to the aggregation of Lewy bodies, the production of dopamine in Substantia Niagara is hindered.Under normal conditions, the protein is dispersed throughout the Substantia Niagara.

FIGURE 2. Lewy bodies in Substantia Niagara
Figure 2 illustrates the aggregation of protein called Lewy bodies in the Substantia Niagara. The Lewy bodies in the Parkinson’s Disease patient hinders the production of the dopamine. Whereas, in normal condition, Lewy bodies are diffused not intervening with production of dopamine. In a study published by L. deLau and M. Breteler, it was observed that Parkinson’s Disease is more prevalent in Europe, North America, and South America . PD is more prevalent in western countries due to common gene strand in Caucasian population. A. Samii, J.G. Nutt, and B. R. Ransom researched the epidemiology of Parkinson’s Disease in depth. The effect of age and bowel movements in increasing the risk of having Parkinson’s Disease was also
studied. The risk of having Parkinson’s Disease increases twice with constant constipation. Age also plays an important factor in increasing the chance of having Parkinson’s Disease . In addition to physiological factors, it is observed that several environmental factors such as pesticide, rural atmosphere, agricultural occupation, water from wells, and overall rural living increases the risk of having PD . The current prototype is especially useful in rural area where availability of clinic is sparse and Parkinson’s Disease is more prevalent.

TABLE 1. Environmental Factors
Table 1 states the environmental factors that increase or decrease the risk of having Parkinson’s Disease. The factors mentioned in the left hand box increase the risk of having PD. Where as, the factors mentioned in the right decrease the risk of having PD. Rural areas have a higher concentration of chemicals and pollen grains, which increases the risk of PD. Exact correlation is not found but it has long been speculated that genetics plays an important role in increasing probability of acquiring PD. The factors decreasing the risk of PD have one thing in common, they produce a brain stimulant. For example, smoking tobacco produces nicotine, a substance that temporarily increases the brain activity. The factors mentioned in the table are speculated to increase or decrease the risk. There are two types of symptoms in Parkinson’s Disease: motor and non-motor symptoms. Jankovic explains four major motor symptoms of Parkinson’s Disease in depth discussed further in Chapter 2 . In an article published by Tjalf Ziemssen and Heinz Reichmann, they discuss in detail the non-motor symptoms such as the olfactory dysfunction (a problem in hearing), sleep disorder, excessive sleep, depression, constipation, and mood disorder. The non-motor symptoms are usually common for several other Parkinsonism related disease. Although, Parkinsonism related disease imitates few symptoms of Parkinson’s Disease, they have entirely different cause for their onset. The non-motor symptoms are not characteristic symptoms for Parkinson’s Disease only. Hence, the non-motor symptom cannot be used for detection and logging of the progress of PD.
Major Motor Symptoms
Parkinson’s Disease has four major motor symptoms and several non-motor symptoms. The majority of the following motor symptoms is researched from the paper published by Jankovic . In addition to the paper by Jankovic, paper published by Samii and associates is also referred .
Bradykinesia
Bradykinesia refers to slowness of movement, a prime feature of Parkinson’s Disease. Reduced firing rates in neurons result in Bradykinesia. As a result of Bradykinesia, a patient may suffer from loss of spontaneous movement, problems in sequencing, overall slowness in movement, difficulty in performing a task with fine motor skills, drooling, loss of expression, decreased arm swing, and decreased blinking .Bradykinesia patients are unable to activate appropriate muscles. Moreover, Electromyography suggests that the patients must produce a burst of agonist, a signal to activate muscles, to fuel the entire movement . Therefore, the Bradykinesia is measured by performing several fast movements with reduced amplitude. Such movements are difficult to produce in PD without external cues. It is difficult to measure the slowness in movement of a person as the slowness varies from person to person. Therefore, it is not advisable to use Bradykinesia for the day to day measurements of PD. Rigidity Rigidity is an increased resistance to the movement of the body parts. Rigidity also means an increased pain in the shoulders, which is often diagnosed as the arthritis. Moreover, rigidity may vary according to age, time, and exercise executed by a person. It is challenging to quantify stiffness in a physical quantity and observe change over a period of time. In summary, rigidity is not a useful symptom for the measurement of Parkinson’s Disease. Postural Deformities and Instability Deformities may occur in the form of abnormal postures (scoliosis), flexed neck, trunk posture, flexed elbows, and knees. It also encompasses the deformity formed in the backbone . The striatal deformities especially occur more often in younger patients. Bent spine, scoliosis, and truncal flexion is worsened by walking. Pisa syndrome is characterized by tilting of the trunk when sitting or standing. Loss of postural reflexes that removes the sense of balance usually occurs in the late stage of Parkinson’s Disease . Hence, loss of postural stability results in falls. For instance, a patient cannot comprehend when the body is moving in the wrong direction or when the body is about to fall. Treatment of dopamine helps in reducing the effect but it is impossible to remove the postural flexion permanently. Albeit, it can be relieved by sitting or sleeping in the supine position. Additionally, leaning against a wall and stretching can help to some extent.
Tremors
Tremors are a highly specific symptom observed in PD and the current project’s backbone. It is observed in the lips, chin, jaw, and legs but rarely in the neck. It possesses a frequency of 4-6 Hz. Sixty-nine percent of patients observed tremors at the onset of PD and 75% during the course of PD. DeLau and Breteler concluded that almost every single patient experienced tremors at some stage of PD . Tremors are both internal and external, and they are experienced both during day and night. Tremors remain consistent from onset to death. Hence, tremors are quantified by measuring acceleration of tremors within the range of resting tremor frequency.
Diagnosis
Historically, one of the best ways to diagnose PD is to detect the presence of Lewy bodies in the Substantia Niagara, which is confirmed by pathology. However, the test is costly and the application of Levodopa to confirm PD can have a devastating effect on the patient who is falsely detected. There are a few symptoms that point to a possible diagnosis of PD. William dauer and Serge Przedborski discusses patients who have a problem working on a task requiring fine motor skills . The person starts to drag a foot due to freezing of gait. This results in problem in walking in a crowded area where constant maneuvers are required. Loss of rhythm is clearly evident when a person is swimming in circles. Moreover, handwriting inches upwards and becomes cramped as it goes towards the end. Additionally, non-motor symptoms are observed such as loss of smell, disturbed sleep due to REM sleep disorder, falling backward often, urinary inconsistency, problems in swallowing, and amnesia . Basic symptoms are first detected such as Bradykinesia, facial expression (immobile or rigid), tremors, and emotions are expressed slowly. A mobile test is performed such as foot tapping and walking as well as repetitive finger tapping for 20 seconds with reduced amplitude. If the patient is 40 years or younger, a tremor is usually observed in the hands or legs. However, if the patient is older than 60 years, they will have a tremor in the chin, jaw, and lips. The important step in determining if the patient has PD is a favorable response to Levodopa.
Tremors
The brain performs an ensemble of essential tasks such as maintaining blood flow, providing a signal to the motor muscles, logical thinking, and interpreting images and noises . Each task is a well-coordinated symphony of signals transferred from a cluster of neurons in the neural network. But, sometimes this symphony is broken due to the misfire or absence of a proper signal transfer in a few neurons, which results in the total or partial breakdown of motor activities. Due to the loss of dopamine, the motor neurons try to compensate by sending signals to each other regularly. As a result, misfired signals from the neuron perform motor activities, which involuntarily cause tremors. Tremors are generally sinusoidal. As the stages progress, the frequency does not change, but the time length and amplitude varies . The tremors observed by Aner Weiss et al. were sinusoidal. Weiss et al. performed the experiment of movement of PD patients to observe the change in their tremors during the movement. Out of all the observed four major symptoms, tremors are one of the most quantifiable and consistent symptoms. Hence, it is possible to measure patient’s progress consistently. Tremors are usually observed at a frequency between 4-6 Hz with a characteristic acceleration produced in each tremor. This frequency measurement makes it a useful criterion for detecting PD . The frequency remains unaltered for tremors; therefore, it is advisable to follow a process to detect tremors for PD detection as it remains unaltered in time and circumstances.