Parkinson’s Disease
James Parkinson described Parkinson’s Disease as a mental disorder that forces body parts into involuntary tremors according to Lorraine V. Kalia and Anthony E. Lang, the leading cause for developing PD is death of dopaminergic neurons in the Substantia Niagara leading to a deficiency of dopamine in the Basal Ganglia.
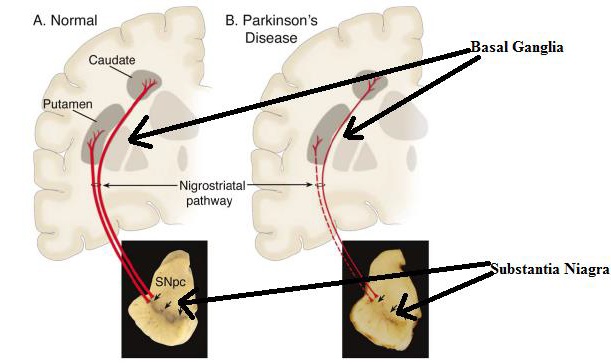
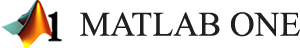
FIGURE 1. Comparison of normal brain and a brain of patient suffering from PD
Figure 1 illustrates the Substantia Nigra and the Basal Ganglia, of a normal person compared to a PD affected patient. Substantia Niagara and the Basal Ganglia are located in middle brain. As observed by Lanneke M.L. deLau and Monique M.B. Breteler, the Substantia Niagara produces the dopamine, which is used by the Basal Ganglia. The Basal Ganglia contains the Putamen and the Caudate, which controls motor functions. The red lines shown in Figure 1 are the nerves transferring dopamine from the Substantia Niagara to the Basal Ganglia. The dotted red line represents the reduced flow of dopamine in patient affected by Parkinson’s Disease. According to the theory proposed by William Dauer and Serge Przedborski, motor neurons will transmit a false signal to various parts of the body. This false signal will produce an involuntary movement with a seemingly fixed frequency. In addition to the involuntary movement the major cause for the onset of Parkinson’s Disease is the collection of protein (brown spot) in Substantia Niagara called Lewy bodies as observed in Figure 2. Due to the aggregation of Lewy bodies, the production of dopamine in Substantia Niagara is hindered. Under normal conditions, the protein is dispersed throughout the Substantia Niagara.
FIGURE 2. Lewy bodies in Substantia Niagara
Figure 2 illustrates the aggregation of protein called Lewy bodies in the Substantia Niagara. The Lewy bodies in the Parkinson’s Disease patient hinders the production of the dopamine. Where as, in normal condition, Lewy bodies are diffused not intervening with production of dopamine. In a study published by L. deLau and M. Breteler, it was observed that Parkinson’s Disease is more prevalent in Europe, North America, and South America. PD is more prevalent in western countries due to common gene strand in Caucasian population. A. Samii, J. G. Nutt, and B. R. Ransom researched the epidemiology of Parkinson’s Disease in depth. The effect of age and bowel movements in increasing the risk of having Parkinson’s Disease was also studied. The risk of having Parkinson’s Disease increases twice with constant constipation. Age also plays an important factor in increasing the chance of having Parkinson’s Disease. In addition to physiological factors, it is observed that several environmental factors such as pesticide, rural atmosphere, agricultural occupation, water from wells, and overall rural living increases the risk of having PD . The current prototype is especially useful in rural area where availability of clinic is sparse and Parkinson’s Disease is more prevalent.

TABLE 1. Environmental Factors
Table 1 states the environmental factors that increase or decrease the risk of having Parkinson’s Disease. The factors mentioned in the left hand box increase the risk of having PD. Whereas, the factors mentioned in the right decrease the risk of having PD. Rural areas have a higher concentration of chemicals and pollen grains, which increases the risk of PD. Exact correlation is not found but it has long been speculated that genetics plays an important role in increasing probability of acquiring PD. The factors decreasing the risk of PD have one thing in common, they produce a brain stimulant. For example, smoking tobacco produces nicotine, a substance that temporarily increases the brain activity. The factors mentioned in the table are speculated to increase or decrease the risk. There are two types of symptoms in Parkinson’s Disease: motor and non-motor symptoms . In an article published by Tjalf Ziemssen and Heinz Reichmann, they discuss in detail the non-motor symptoms such as the olfactory dysfunction (a problem in hearing), sleep disorder, excessive sleep, depression, constipation, and mood disorder. The non-motor symptoms are usually common for several other Parkinsonism related disease. Although, Parkinsonism related disease imitates few symptoms of Parkinson’s Disease, they have entirely different cause for their onset . The non-motor symptoms are not characteristic symptoms for Parkinson’s Disease only. Hence, the non-motor symptom cannot be used for detection and logging of the progress of PD.