Obesity and Heart Failure
Obesity is defined as abnormal or excessive fat accumulation that presents a risk to health. (Carbone 2013) Currently, obesity is defined based on the Body Mass Index (BMI), which relates height to weight. A BMI greater than or equal to 30 kg/m2 defines obesity. According to this criterion, more than 35% of the USA population is considered obese. With HF being a disease associated with many co-morbidities, obesity is commonly seen in HFpEF. During obesity, there is adipose tissue dysfunction, so called “adiposopathy”, which is a proinflammatory state and adversely affects metabolism and cardiovascular function via autocrine, paracrine or endocrine mechanisms. The effects of adipokines secreted by adipose tissue on the cardiovascular system have been widely described. Accelerated CAD is associated with an adipokine imbalance with increased expression and secretion of pro-inflammatory adipokines such as TNFα, leptin and MCP-1, whilst anti-inflammatory adipokines such as adiponectin (APN) are decreased (Tilg and Moschen 2006; Van de Voorde et al. 2013; Ouchi et al. 2011; Gualillo, González-Juanatey, and Lago 2007; Romacho et al. 2014). Many other mechanisms have been proposed to explain how obesity leads to heart failure, some of them are demonstrated in Figure 1 showing alterations in blood volume leading up hemodynamic alterations which eventually induce cardiac structural abnormalities.
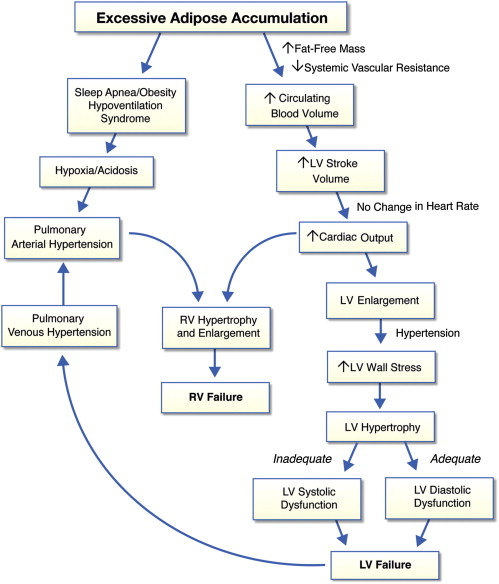
Figure 2. Pathophysiology of Obesity Cardiomyopathy
This figure shows the central hemodynamic, cardiac structural abnormalities and alterations in ventricular function that may occur in severely obese patients and predispose them to heart failure. In severely obese patients presenting with systemic hypertension, concentric LV hypertrophy is more frequently observed which leads to diastolic heart failure. Figure taken from Lavie et al. 2013.