Neural Mechanisms behind Migraine Photophobia
Photophobia specifies light-induced neurological symptoms including exacerbation of headache, hypersensitivity to light, and ocular discomfort/pain (photo-oculodynia) (Noseda & Burstein, 2013). Thus, ambient light exposure aggravates the perception of migraine headache (Kawasaki & Purvin, 2002; Liveing, 1872) and is experienced by about 90% of migraineurs with normal eyesight (Liveing, 1872; Selby & Lance, 1960; Drummond, 1986). Observations in blind migraine patients indicates that photophobia is reliant on photic signals from the eye that synapse with TGV neurons somewhere along its path (Noseda & Burstein, 2013). Migraine patients who do not have visual perception due to complete optic nerve damage testify that light does not hurt them during a migraine attack, their sleep cycle is irregular, and light does not induce pupillary response. wever, headache exacerbation is still experienced in blind migraineurs with intact optic nerve and partial light perception, but have no sight because of severe degeneration of rod and cone photoreceptors (Noseda et al., 2010a). Retinal projections are composed of two physiologically different routes to the brain. One pathway forms images by photoactivation of rods and cones (Noseda & Burstein, 2013). The other regulates biological functions like pupillary reflex, circadian photoentrainment, and melatonin release by activating photosensitive retinal ganglion cells containing melanopsin photoreceptors (Klein & Weller, 1972; Freedman et al., 1999; Lucas et al., 2001). All retinal photoreceptors presumably contribute to migrainetype photophobia in migraineurs with normal eyesight (Noseda & Burstein, 2013). The speculated neural mechanism for headache exacerbation is the convergence of photic signals from retina onto TGV thalamo-cortical pathway (Noseda et al., 2010a). Light heightens thalamic TGV neuron activation. Also, retinal ganglion cells directly transmit signals to a subgroup of neurons sensitive to light/dura that are situated in the posterior thalamus. The axonal projections of these neurons lead to cortical areas associated with pain processing and visual perception. A mechanism for photo-hypersensitivity proposes that TGV nociceptive signals during a migraine attack enter the visual cortex through the light/dura-sensitive neurons in the posterior thalamus which then responds differently to visual stimuli and becomes hyperexcitable in migraineurs. However, TGV nociception may not be the only pathway to contribute to visual cortex hyperexcitability since this hyperexcitability persisted during a migraine attack and after headache relief, but not during the interictal period (Denuelle et al., 2011). Photo-oculodynia could come from indirect activation of a pathway that includes the olivary pretectal nucleus, SSN, and sphenopalatine ganglion (Okamoto et al., 2010).
These areas parasympathetically regulate vasodilation and mechanical changes in ocular blood vessels. These responses activate trigeminal nociceptors and second ordernociceptive neurons in spinal trigeminal nucleus. Yet, there is no evidence that light evokes vasodilation in the human retina (Noseda & Burstein, 2013).
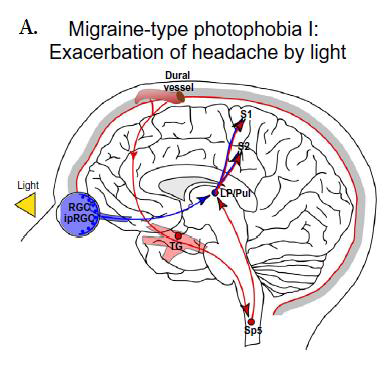


Figure 1. Photophobia Mechanism. Proposed mechanisms for A) exacerbation of headache by light, B) light hypersensitivity in migraineurs, and C) light-induced ocular pain (Noseda & Burstein, 2013).
