Improvement of surgery duration estimation
The United States health care industry currently faces numerous challenges. In an era of changes, the system faces rising costs and increased demand for its services. This is a result of an aging population and the newly enforced Affordable Care Act. The Affordable Care Act, signed into law on March 23, 2010, is a federal statue aimed to improve the U.S. health care system. The goal is to make services accessible to all Americans, increase the benefit from insurance and use of the services, and reduce overall spending. One way the act works to achieve this goal is by expanding Medicaid, the federal-state funded program, to provide financial aid for medical services to low-income citizens . As a whole, the Affordable Care Act is expected to increase the number of insured citizens by 33 million. This creates an increased demand for health services and places a larger strain on the providers. In the United States, the healthcare industry accounts for 17.9% of the GDP as total healthcare spending exceeded $2.6 trillion in 2010 . “The amount of public money needed to finance health care, which currently stands at 45% of all health care expenditures, is expected to double by 2050 . In 2009, $130 billion dollars was spent due to inefficiently delivered services . These costs, paired with an increase in health care demand, motivate the industry to improve system operations. As the industry changes, providers are facing increasing competition. For example, statistics on costs of surgeries are available to the public, making it possible for people to shop around if they are not satisfied. Furthermore, patients are increasingly traveling abroad for advanced and less expensive medical procedures .
Statical Methods For Surgery Duration Estimation
Surgery is a primary source of revenue in a hospital, and scheduling of surgery largely drives that revenue. A key challenge in creating schedules that minimize the amount of waiting time for patients and maximize the utilization of the operating rooms is accurately estimating surgery durations. Using data from a large Midwestern hospital, surgery duration estimations were compared to actual durations in a one-year period for the top surgeries. Statistically, a significant difference between actual and estimated durations was proven. With the goal of decreasing the difference between the estimated and actual durations, multiple linear regression models were created for the most common surgeries and used to analyze the impact various characteristics of surgery cases have on the duration. Due to the high variability of the data, the regression method was not found particularly useful in identifying strong correlations in the input characteristics.
Introduction
For hospitals, surgery is a vital source of revenue. It is estimated that 40% of a hospital’s costs and 68% of its revenue come from surgery . As health care costs rise in the United States , improving the efficiency of surgery scheduling has become an area of focus for both providers and researchers. Technological capabilities within surgery scheduling have been improving as well, utilizing an array of software programs to record surgery data and use it as a tool to schedule future surgeries. When scheduling surgery, hospitals must take into account the needs of patients and surgeons, as well as their own budgets. This can be a significant challenge, as these needs include patients’ requests, surgeons’ schedules, and hospital resource availability. According to the Centers for Medicare and Medicaid Services, data on the costs of surgery to the patient are readily available to the public. This allows patients to compare costs across hospitals in the region, and gives them the knowledge that can drive their choice to have surgery at another location if they are not satisfied with prior experiences. Surgeons can also send their services and patients elsewhere if they are not satisfied themselves with the services provided by the hospital, such as the way the surgeries are scheduled or the way their requests are handled. A hospital must meet its own financial needs as well, ensuring that the necessary utilization of their resources is met. These priorities are a challenge to balance, as they often conflict.
Comparison of Estimated and Actual Surgery Durations
The biggest challenge Unity Point Health’s surgery schedulers face is estimating surgery durations. Current practice is to ask the surgeons to estimate the time the case is going to take and then add a fixed amount of time for cleanup. This is consistent with Broka et al. . These estimations are not limited to sets of a certain number, but they tend to be rounded to the next five minute increment. The estimate given by the surgeon is compared to the average for the last ten surgeries for that procedure type and surgeon, given in the electronic medical record database. If the surgeon’s estimate is significantly different, the specialty team leader will look into the reason why and make a decision on the final estimate. In the one year period, the surgery cases started late 80% of the time and started exactly on time 1.4% of the time. To further assess the magnitude of this problem, t tests were used to compare estimated duration versus actual times of surgeries. The top four surgeries by count were evaluated, both for all of the surgeons collectively and each of the top surgeons separately. We defined the top surgeons as those that performed at least 10% of the total number of cases done with that procedure. The procedures evaluated were Laparoscopic Cholecystectomy (Lap Chol), Esophagogastrodueodenoscopy (Esophag), Cystoscopy (Cyst), and Insert Port Vascular Access (IPVA). Lapraroscopic Appendectomy (Lap App) was also a top surgery, but was not evaluated because 64% of the cases are emergency procedures, and therefore were not scheduled in the surgery scheduling process. These five procedure types make up 9.3% of the total surgeries performed in that span of time. Because the estimates were based on historical data, the surgeons did not know the estimates were being analyzed, eliminating a source of bias. For our purposes, we eliminated data points that were not complete and assumed the rest of the data was recorded accurately. The emergency surgeries were also eliminated, as they were not estimated using the same process as the elective surgeries. Twenty minutes were subtracted from each estimated time to account for the cleanup time the schedulers added in. The actual time does not include the cleanup time. Significant outliers, defined as those greater than six times the standard deviation (6σ) were removed. The results of the t test are shown in Table 1.
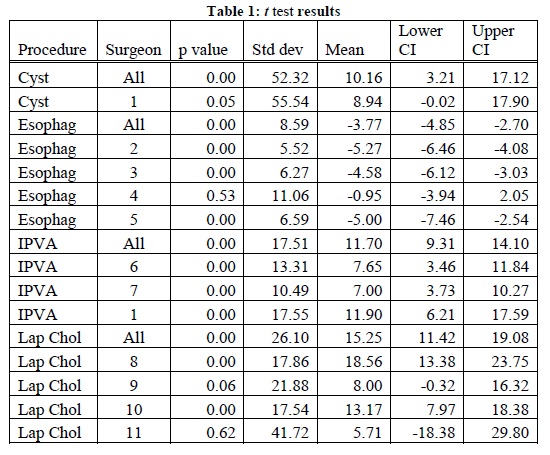
Table 1: t test results
Impact of Variables Using Multiple Linear Regression
Factors affecting how long a surgery takes vary immensely. In order to evaluate the impact of these factors, multiple linear regression was used. The same one year period of historical data was analyzed, looking at the procedure start to procedure end time as the dependent variable, as well as the corresponding information for the independent variables. The procedure time does not include anesthesia time or cleanup time, and therefore eliminates sources of variability. A model was created for each of the top four surgeries by count and the surgeons who make up at least 10% of the cases for that procedure in the data acquired. In this case, Lap App was included and Cyst was not. Even though 64% of the Lap App cases were emergency, there is no reason to think the durations are affected by the variables looked into differently than non-emergency cases. Cyst was not used in the regression model because of its high standard deviation compared to the other procedure types .