Hypertension and HFpEF
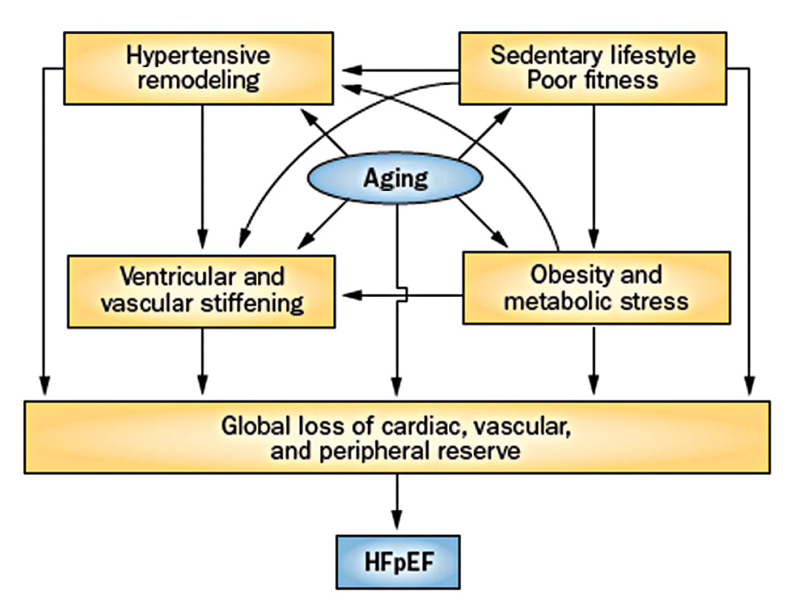
HFpEF is a complex disease often presenting with multisystem involvement characteristics including skeletal muscle and vascular dysfunction, pulmonary hypertension, renal failure, anemia, and atrial fibrillation. (Maeder and Kaye 2009) The prevalence of HFpEF compared to HFrEF is rising at an alarming rate of 1% per year, which is rapidly turning HFpEF into the most prevalent HF phenotype with little to no improvement in outcome. (Owan et al. 2006) Since obesity and hypertension occur often together, we studied hypertension as a cause of HFpEF. HFpEF is associated with relative increases in aldosterone levels so the Sam lab developed a murine model of hypertension induced HFpEF through chronic aldosterone infusion. Aldosterone contributes greatly to the development of hypertension. This role has been supported by numerous cross-sectional studies relating plasma aldosterone level to ambulatory blood pressure (BP) measurements. (Calhoun 2006) It is further supported by the antihypertensive efficacy of aldosterone antagonists in treating hypertension. Both HFpEF and HFrEF are associated with systemic and cardiac activation of the renin-angiotensin-aldosterone system (RAAS). Aldosterone levels have been shown to be significantly elevated in HF patients. Aldosterone is involved in the inflammatory response and cause myocyte hypertrophy, death, apoptosis, and altered protein expression of enzymes in the oxidation pathway of long chain fatty acid and reactive oxygen species in both in vivo and in vitro models. Aldosterone is also produced in the heart and is responsible for mediating cardiac remodeling and fibrosis. (Silvestre et al. 1998). These evidences led to testing of anti-aldosterone treatments such as spironolactone for HFpEF. During the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) trial, spironolactone, a mineralocorticoid receptor blocker, was used to treat patients with HFpEF. Despite being able to reduce diastolic dysfunction parameters in these patients, spironolactone was not able to significantly reduce the composite primary end point of death from cardiovascular causes, aborted cardiac arrest, or hospitalization for heart failure. (Pitt et al. 2014) This led us to address other possible mechanisms for the treatment of HFpEF.
Hypertension and HFpEF