The healing of bone grafts
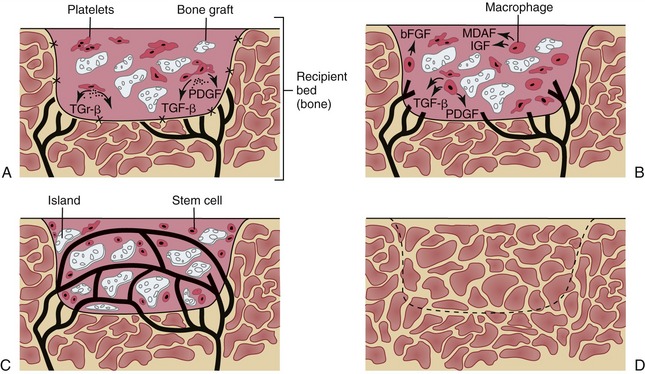
Bone is a unique connective tissue in that it heals and remodels by cellular regeneration rather than scar formation. This cellular regeneration makes the nonvascularized bone grafts possible. The immature mesenchymal stem cells can differentiate into different tissues e.g. bone, muscle, cartilage, and fibrous tissues. In bone, they are located in the bone marrow, endosteum, and the cambium layer of the periosteum. The number of these cells have been found to decrease with age making the bone more osteoperotic and less regenerative.Bone formation occur by three mechanisms: 1) Osteogenesis by forming new bone from stem cells; 2) Osteoconduction by forming new bone from host-derived or transplanted stem cells along biologic or alloplastic framework; 3) Osteoinduction by the guided differentiation of progenitor stem cells into bone forming cells “osteoblasts” by bone inductive proteins (e.g. bone morphogenic proteins “BMP”). Cancellous nonvascularized bone graft cells initially survive by the plasmatic circulation. Lactic acid build-up and hypoxia initiates the formation of new blood vessels from the surrounding tissues, which is usually completed around two weeks. The surviving progenitor cells form unorganized woven bone (phase 1 bone). Over the next few months, remodeling occurs to form the lamellar structure of the one (phase 2 bone). Vascularized free flap has the advantage of transferring a viable bone with its cells thus bypassing the need for bone formation across the continuity defect. The only exception to that is at the graft-mandible and graft-graft interfaces. The healing along these gaps has not been studied specifically but it is fair to assume that bone formation along these gaps occurs by osteogenesis, osteoinduction, and / or osteoconduction. Clinical experience also showed that healing along these gaps might result in fibrous tissue formation rather that true bony healing in some cases. This may be a result of the initial size of the gap, type of fixation, systemic host factors, radiotherapy or a combination. This study is intended to develop a reliable technique to assess bone formation along these gaps. This can be utilized in future studies to identify factors affecting the healing along these gaps.
The healing of bone grafts

